Every winter, the wellness industry floods our feeds with products promising to “boost” our immune systems into superhero status. Supplements, superfoods, and exotic botanicals compete for attention with increasingly bold claims about disease prevention. This marketing language reveals a fundamental misunderstanding of human immunology. You do not actually want a boosted immune system. An overactive immune response produces allergies, autoimmune conditions, and the chronic inflammation underlying most modern diseases. What you want is an immune system that remains primed, appropriately responsive, and properly regulated.
True immune resilience cannot be found in any single powder, pill, or protocol. It emerges from a hierarchy of physiological needs that begins with lifestyle foundations and extends through targeted nutritional support. The distinction matters because it determines where your investment of time and money will produce genuine returns versus placebo effects and expensive urine.
Research from the National Institutes of Health and the European Journal of Clinical Nutrition consistently demonstrates that immune function depends on the interaction of multiple systems: sleep architecture, nutritional status, stress physiology, and physical activity patterns. Optimizing one while neglecting others produces limited benefit. The protocol outlined below addresses these systems in order of impact, helping you distinguish between marketing hype and biological reality as we enter the peak of respiratory virus season.
The Foundation: Sleep as the Master Regulator
Before spending a single dollar on supplements, you must audit your sleep. This isn’t motivational advice or wellness platitude. Sleep is the period when your immune system performs its most critical maintenance, surveillance, and memory consolidation functions. During deep slow-wave sleep, your body releases cytokines, signaling proteins that help coordinate immune responses against pathogens and cellular damage. Sleep deprivation doesn’t merely make you tired; it actively dismantles immune defenses.
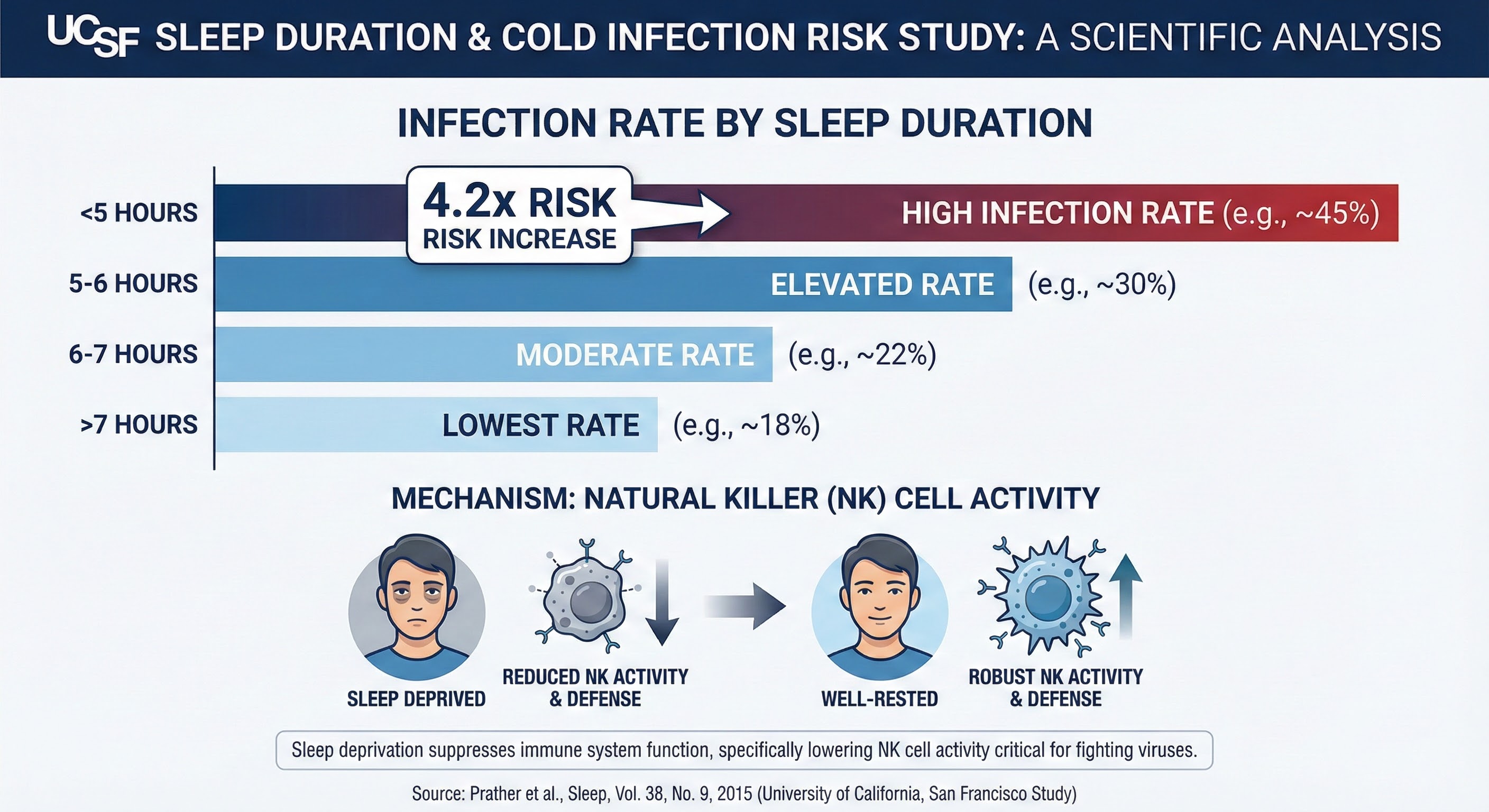
The research on this relationship is remarkably consistent. A landmark study from the University of California, San Francisco, published in Sleep, found that people who slept less than six hours nightly were 4.2 times more likely to develop cold symptoms when exposed to rhinovirus compared to those who slept more than seven hours. The relationship held after controlling for pre-existing antibody levels, age, body mass, smoking, alcohol use, and even subjective sleep quality. Actual sleep duration predicted infection independent of all other measured factors.
Dr. Matthew Walker’s research at UC Berkeley has further demonstrated that a single night of four hours sleep reduces natural killer cell activity by approximately 70% the following day. Natural killer cells represent your immune system’s first-line surveillance against viral infections and cancerous cells. Their dramatic suppression from acute sleep loss explains the increased susceptibility to infection that exhausted individuals experience.
No supplement can compensate for chronic sleep debt. A strict seven-to-eight-hour sleep window represents your primary line of immune defense, more important than any pill in your medicine cabinet. If you’re sleeping six hours or less and wondering why you catch every virus circulating through your office, the answer isn’t zinc deficiency. For those struggling with winter sleep disruption, our guide on light therapy protocols for short days addresses the circadian challenges that undermine sleep quality during dark months.
The Nutrient Tier: Filling Modern Gaps
Once sleep is optimized, we turn to micronutrients. The immune system requires specific vitamins and minerals to generate cells, produce antibodies, and mount appropriate inflammatory responses. Deficiencies in key nutrients create genuine vulnerabilities, but the relationship isn’t linear. Immune function follows a U-shaped curve regarding nutritional status: too little impairs response capacity, but too much can prove immunosuppressive or pro-inflammatory.
The goal of supplementation should be filling gaps left by modern diets and lifestyles rather than overwhelming the body with megadoses that may blunt beneficial hormetic signaling. Most people in Western societies aren’t overtly malnourished by traditional definitions. They consume adequate calories. However, they are often sub-clinically insufficient in specific micronutrients required for optimal immune cell proliferation and function. Addressing these specific insufficiencies restores the immune system’s capacity to respond appropriately to threats.
Vitamin D is technically a prohormone rather than a vitamin, and it modulates the expression of over 1,000 genes, including dozens governing immune response. Vitamin D receptors appear on virtually every immune cell type. During winter months, especially above the 37th parallel, UV exposure is insufficient to maintain optimal serum levels regardless of time spent outdoors. The sun’s angle simply doesn’t allow adequate UVB penetration to trigger dermal synthesis.
Target blood levels between 40 and 60 ng/mL, which typically requires supplementation of 2,000 to 5,000 IU daily depending on baseline status, body composition, and individual absorption. Take vitamin D with dietary fat to enhance absorption, and consider adding vitamin K2 (MK-7 form) to direct calcium toward bones rather than soft tissues. A 2020 meta-analysis in The Lancet Diabetes & Endocrinology found that vitamin D supplementation reduced acute respiratory infection risk by 12% overall, with effects reaching 70% reduction in those with severe baseline deficiency.
Zinc is crucial for the development and function of immune cells including neutrophils, macrophages, and natural killer cells. It also demonstrates direct antiviral properties, particularly in preventing viral replication in the nasopharyngeal mucosa. This is why zinc lozenges, which dissolve slowly in the mouth, show stronger effects than zinc capsules swallowed into the stomach.
For prophylactic use during high-risk periods, aim for 15 to 30 mg elemental zinc daily from food and supplements combined. Zinc acetate or gluconate lozenges are preferred forms for upper respiratory protection. Avoid zinc picolinate or citrate in lozenge form, as these chelated forms don’t release ionic zinc effectively in the throat. Long-term supplementation above 50 mg daily can induce copper deficiency, so moderate dosing matters.
Vitamin C functions more as a support player than the cure-all it’s sometimes marketed as. It accumulates in phagocytes and enhances their oxidative burst capacity against pathogens. Research suggests vitamin C doesn’t prevent colds in the general population, but it may shorten duration by approximately 8% in adults and 14% in children. Since your body cannot store vitamin C beyond tissue saturation, consuming smaller doses of 200 to 500 mg throughout the day proves more effective than single large doses that largely end up in urine.

Environmental Control: The Overlooked Factor
We obsess over what we put into our bodies while largely ignoring the air around us. Yet environmental factors profoundly influence both pathogen exposure and immune barrier integrity. Winter conditions create a perfect storm of increased viral transmission and compromised mucosal defenses that supplements alone cannot overcome.
Indoor air during winter is naturally dry, and central heating systems exacerbate the problem dramatically. Relative humidity below 40% causes the mucous membranes lining your nasal passages and throat to dry out, creating microscopic cracks in your physical barrier against airborne pathogens. These mucosal surfaces are your first line of defense; when compromised, viruses that would otherwise be trapped and expelled gain direct access to respiratory epithelium.
Research from Yale University, published in PNAS, demonstrated that low humidity impairs mucociliary clearance, reduces interferon signaling in response to viral infection, and increases the viability of aerosolized viruses. The investigators found that mice housed in 10-20% relative humidity developed significantly more severe influenza infections than those in 50% humidity, even when exposed to identical viral loads. The dry air created vulnerability at every level of immune defense.
The practical intervention is straightforward: use a cool-mist humidifier in your bedroom to maintain humidity between 40 and 50 percent. Monitor levels with an inexpensive hygrometer. Be aware that humidifiers require regular cleaning to prevent mold and bacterial growth that would introduce new problems.
Ventilation also matters. Even when cold, crack a window for 10 to 15 minutes daily to flush out accumulated CO2 and stale air. Indoor spaces with poor ventilation accumulate higher concentrations of viral particles when infected individuals are present. The dilution effect of fresh air reduces exposure intensity, and some research suggests that the air exchange itself may be more protective than most air purification systems.
The Exercise Sweet Spot
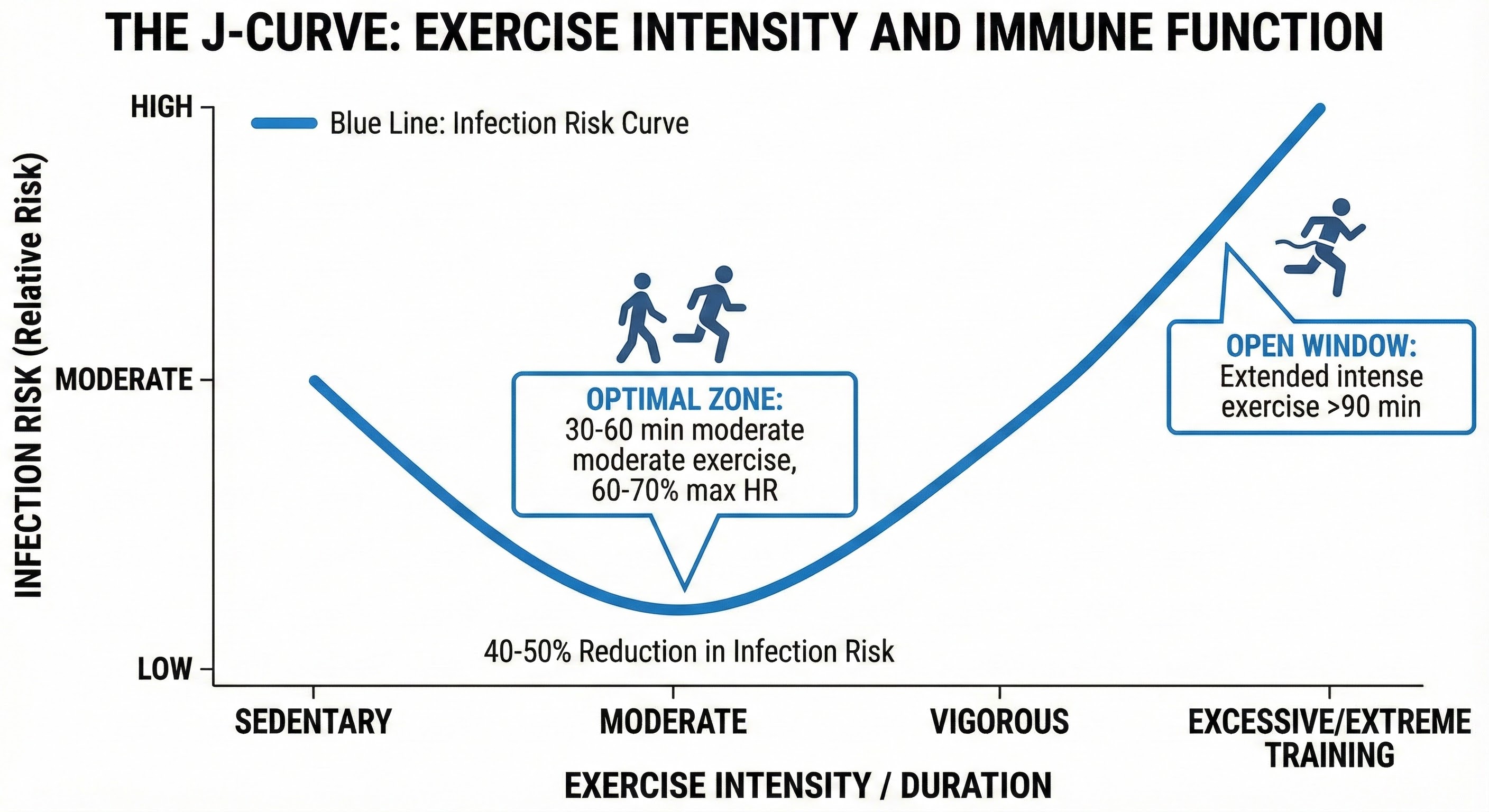
Physical activity demonstrates a J-shaped relationship with immune function. Moderate, consistent exercise improves the circulation and surveillance efficiency of immune cells, reduces chronic inflammation, and enhances stress resilience. However, prolonged, high-intensity exertion without adequate recovery can temporarily create an “open window” of immune suppression lasting several hours to days.
Research from Appalachian State University found that 30 to 60 minutes of moderate exercise, defined as 60 to 70 percent of maximum heart rate, performed regularly reduces upper respiratory infection incidence by approximately 40 to 50 percent compared to sedentary individuals. The mechanism involves enhanced circulation of neutrophils, natural killer cells, and T cells during and immediately following exercise, along with anti-inflammatory effects of myokines released from contracting muscles.
The vulnerability window appears after prolonged intense efforts exceeding 90 minutes at high intensity, particularly when combined with other stressors like inadequate sleep, caloric restriction, or psychological strain. Marathon runners, for example, show elevated infection rates in the weeks following races. This doesn’t mean avoiding hard training; it means timing intense efforts when other stress factors are managed and ensuring adequate recovery nutrition and sleep.
If you’re already feeling run down with early symptoms, this is not the time to attempt personal records. Zone 2 cardio or a light strength session stimulates immune circulation without creating additional systemic stress. A practical guideline: if symptoms are “above the neck” only, such as runny nose or mild congestion, light movement is usually tolerable. If symptoms include anything “below the neck,” including body aches, chest congestion, or fever, rest is the only evidence-based prescription. Our guide on holiday workout routines offers efficient protocols for maintaining fitness without the overreaching that suppresses immunity.
Stress and the Gut-Immune Axis
Chronic psychological stress exerts profound immunosuppressive effects through cortisol elevation and sympathetic nervous system activation. While acute stress temporarily enhances certain immune parameters, preparing the body for potential injury, chronic stress produces the opposite effect. Sustained cortisol elevation reduces lymphocyte counts, impairs antibody production, and shifts immune function toward inflammatory rather than antiviral responses.
The gut-immune connection adds another dimension. Approximately 70% of immune tissue resides in the gut-associated lymphoid tissue (GALT), where it samples antigens from digested food and resident microbiota. Chronic stress disrupts intestinal barrier integrity, increases gut permeability, and alters microbiome composition in ways that promote inflammation and impair immune regulation.
Practical stress management need not involve meditation retreats or extensive protocols. Even brief interventions show benefit. A 2019 study in Psychoneuroendocrinology found that three minutes of slow, deep breathing (six breaths per minute) shifted autonomic balance toward parasympathetic dominance and reduced cortisol levels in subsequent hours. Regular brief practices likely provide greater cumulative benefit than occasional long sessions.
Social connection also modulates immune function through stress pathways. Research from Carnegie Mellon University demonstrated that individuals with diverse social networks showed increased resistance to experimentally introduced cold viruses, independent of the antibody levels they developed. The mechanism appears to involve reduced cortisol and enhanced positive affect that accompanies social integration.
The Bottom Line
Immune health is an investment built through consistent daily practices, not a lottery ticket purchased through emergency supplement runs when you feel symptoms emerging. The hierarchy is clear: optimize sleep as the non-negotiable foundation, address specific nutrient insufficiencies common to modern life, manage environmental factors that compromise barriers, maintain moderate physical activity, and attend to stress and social connection.
You cannot ignore these fundamentals for eleven months and expect any supplement to rescue you in December. The marketing promises of immune “boosting” products exploit both our anxiety about illness and our desire for simple solutions. True immune resilience doesn’t come in a bottle. It emerges from the accumulated effect of how you sleep, eat, move, and connect across weeks and months.
Your Daily Immune Protocol:
- Protect 7.5 to 8 hours of sleep as your primary immune investment
- Maintain bedroom humidity at 40 to 50 percent during winter months
- Supplement vitamin D3 (2,000-5,000 IU daily) with vitamin K2, targeting blood levels of 40-60 ng/mL
- Keep zinc lozenges available for acute use at first sign of throat symptoms
- Exercise moderately for 30 to 60 minutes most days; reduce intensity when feeling run down
- Practice brief stress management daily: even three minutes of slow breathing shifts immune function
Sources: Sleep journal UCSF study on sleep and cold susceptibility, UC Berkeley natural killer cell research (Dr. Matthew Walker), The Lancet Diabetes & Endocrinology vitamin D meta-analysis (2020), Yale University humidity and influenza research (PNAS), Appalachian State University exercise immunology studies, Carnegie Mellon University social network and infection resistance research, Psychoneuroendocrinology breathing and cortisol studies (2019).